Shingles: The Painful Virus That Can Complicate Your Life

Shingles, also known as herpes zoster, is a viral infection caused by the reactivation of the Varicella Zoster virus, which also causes chickenpox. After a person has chickenpox, the virus remains dormant in the body, hiding in nerve tissues near the spine and brain. Shingles occur when this virus is reactivated, most often in older adults or individuals with weakened immune systems.
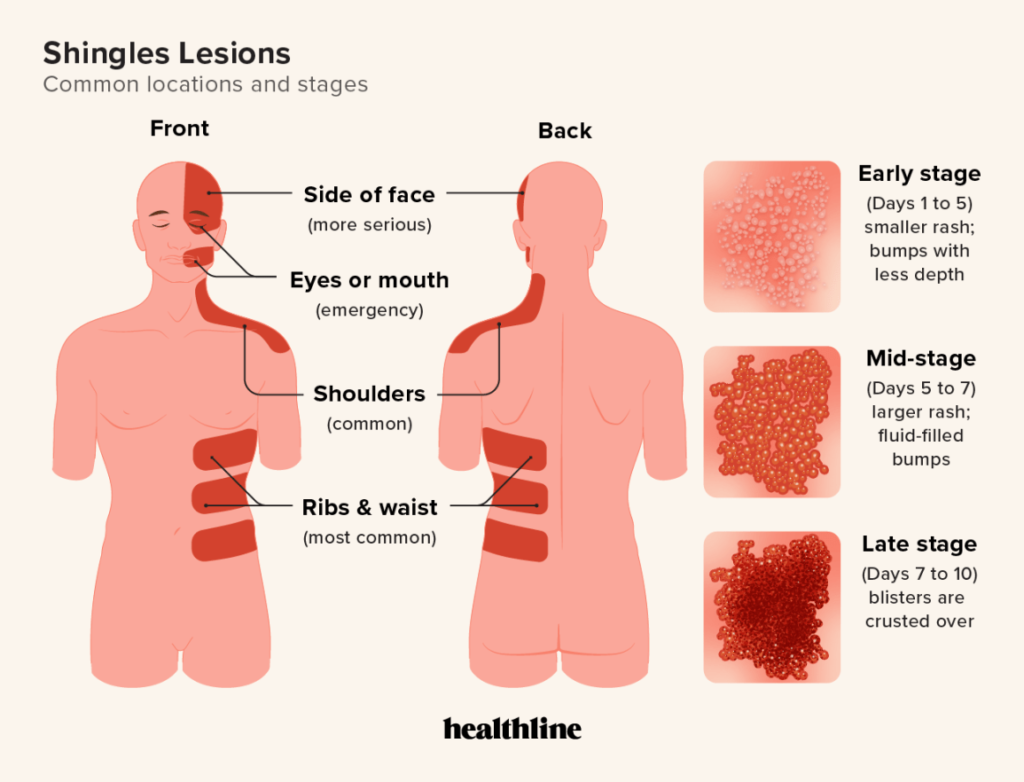
Where do shingles occur and how do they look?
Shingles manifest along the pathways of the affected nerves, which is linked to the fact that the chickenpox virus resides in nerve tissue and then activates, causing infection in that area.
- Unilateral localization: The rash is usually confined to one side of the body, which is an important diagnostic feature. Once awakened, the virus spreads along the nerve endings, explaining the unilateral nature of the rash.
- Rash distribution: It often occurs along the ribs (on the chest) or on the face, following the path of the affected nerve. It affects dermatomes—skin areas innervated by specific nerves—resulting in a characteristic band-like rash. This is due to the virus activating in one of the nerve ganglia and spreading along the nerve fibre.
Ganglia (or nerve nodes) are groups of nerve cells located outside the central nervous system. They serve as “crossroads”; for nerve pathways, where sensory or motor signals are transmitted and processed.
Risk Factors for Shingles
As people age, their immune systems naturally weaken, making the body more vulnerable to viral infections.
- Age: Individuals over 50 years old are at a higher risk.
- Weakened Immune System: Those with compromised immune systems, such as individuals with HIV, cancer, undergoing steroid therapy, or with chronic illnesses (like diabetes, cardiovascular diseases, and autoimmune disorders), are also at risk.
- Stress: Physical or emotional stress can play a role in the reactivation of the virus.
- Sleep and Daily Routine: Sleep disturbances and lack of rest negatively affect immunity, increasing the likelihood of shingles outbreaks.
- Nutritional Deficiencies:
- A deficiency in vitamin D is associated with more frequent shingles outbreaks. This vitamin plays a key role in immune function, and low levels can weaken the body’s defences against viruses.
- Insufficient vitamin B12 can worsen shingles symptoms and delay recovery.
- A lack of antioxidants (such as glutathione, vitamins C and E) may also increase risk, as they support skin health and immune cells.
- Infections: Any serious infections can trigger a shingles outbreak by weakening the immune system and/or activating nerve cells where the virus can “sleep”; Many cases of viral reactivation occurred during the pandemic.
- Nerve Trauma: Including surgical interventions or inflammation can lead to the reactivation of the virus in damaged nerves.
These factors collectively significantly influence the likelihood of shingles outbreaks. Research emphasizes the importance of maintaining a strong immune system and managing stress to reduce the risk of recurrences.
Complications of Shingles
The complications of shingles can vary and affect different organs and systems. Here are the main complications:
- Postherpetic Neuralgia (PHN): This is the most common complication, characterized by persistent pain in the area where the rash occurred, even after it has resolved. About 10-15% of patients experience PHN, and the risk increases with age. The pain can be severe, burning, or stabbing, significantly impacting the quality of life and causing difficulties in daily activities.
- Vision and Hearing Problems: If the rash is located near the eyes or ears, it can lead to serious complications such as:
- Vision Loss: Eye involvement can result in blindness if treatment is not initiated promptly.
- Hearing and Vestibular Issues: The virus can damage the auditory nerve or lead to vestibular disorders, causing hearing loss, dizziness, and tinnitus.
- Bacterial Skin Infections: Damaged skin can become an entry point for bacterial infections, especially if blisters break and form open wounds. This may require antibiotic treatment to prevent further complications, such as abscesses.
- Oral Cavity Lesions: Less commonly, shingles can affect the mucous membranes in the mouth, making it difficult to eat, swallow, or speak.
Severe Complications
- Facial Rashes, especially in the eye area, can lead to severe complications, such as facial muscle paralysis and encephalitis.
- Involvement of the face or eyes increases the risk of stroke or meningitis.
Immediate medical attention is necessary if rashes appear on the face or eyes.
How Does the Rash Progress?
The rash associated with shingles goes through several stages:
- Prodromal Symptoms (1-5 days): Before the rash appears, there may be sensations of tingling, burning, or itching in specific areas of the body due to the virus irritating nerve endings.
- Initial Rash Stage (1-2 days): After a few days, red spots appear that quickly develop into small fluid-filled blisters. These blisters cluster on one side of the body, typically along dermatomes.
- Vesicular Phase (5-7 days): The blisters begin to fill with clear or cloudy fluid, and their surfaces may rupture, increasing the risk of spreading the virus (until the fluid in the blisters has dried).
- Crusting Stage (7-10 days): The blisters dry out and form crusts that gradually fall off. At this stage, the rash is no longer contagious.
- Healing (2-4 weeks): In most cases, the rash completely resolves within 2-4 weeks, but some individuals may be left with scarring on the skin. In addition to skin manifestations, many patients continue to experience nerve pain.Bottom of Form
https://www.healthline.com/health/shingles-lesions
How the Virus Spreads
The varicella-zoster virus (VZV), which causes shingles, can be transmitted from person to person, but with an important clarification: shingles itself is not contagious. However, the virus can be passed on to individuals who have never had chickenpox. Infection occurs through direct contact with the fluid that leaks from the blisters of the rash.
Individuals with an active shingles rash can transmit the virus to others, potentially causing chickenpox (but not shingles) in those who have never been infected. This can happen until the rash has crusted over.
People with active shingles should avoid contact with:
- Pregnant women who are not immune to chickenpox.
- Infants and children who have not had chickenpox or have not been vaccinated.
- Individuals with weakened immune systems, as they are at a higher risk for serious complications.
Direct contact with the fluid from the blisters is the primary route of transmission, so it’s advisable for everyone to avoid contact with the rash.
When to Seek Medical Attention
- If the rash involves the face or eyes, this can lead to serious complications like blindness or hearing loss.
- If the pain becomes unbearable or worsens, even after treatment has begun.
- If there are signs of a bacterial infection, such as redness, pus, or swelling in the affected area.
Treatment of Shingles
- Antiviral Medications: These medications are effective in reducing the duration and severity of the illness, especially if started within the first 72 hours after symptom onset. Antivirals can help prevent complications, such as postherpetic neuralgia.
- Pain Relief: Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may be prescribed to alleviate pain.
- Skin Care: Proper care of the rash is recommended to prevent infection and promote healing. This includes:
- Keep the affected area clean and dry.
- Use bandages to protect from injury and prevent infection.
- Avoid scratching the rash, as this can lead to bacterial infections.
Prevention of Shingles Flare-Ups
Preventing flare-ups of shingles involves several important aspects that can help prevent recurrences and improve recovery after the illness:
- Local injections of vitamin B12 near the nerves affected by the virus:
- During an outbreak: Vitamin B12 may be particularly beneficial during pronounced neurological symptoms, such as pain and numbness. It helps maintain nerve cells and reduces the risk of postherpetic neuralgia.
- Between outbreaks: Regular B12 injections during remission can strengthen nerves and prevent further complications, especially in patients with chronic vitamin deficiencies.
- Use of antioxidants: Antioxidants such as glutathione, and vitamins C and E can support the immune system and help repair cells after viral damage. They protect cells from oxidative stress and promote tissue healing.
- Diet: A balanced diet focusing on foods rich in vitamins, minerals, and antioxidants can help maintain immunity and speed up recovery. Foods high in lysine (e.g., fish, eggs, dairy) may be beneficial in suppressing the virus, while those rich in arginine (e.g., chocolate, nuts) should be limited, as they may promote viral activity.
- Healthy lifestyle: Maintaining a healthy lifestyle—regular physical activity, good sleep, stress management, and avoiding harmful habits (such as smoking)—is also essential in preventing shingles recurrences. Chronic stress and a weakened immune system can increase the likelihood of virus activation.
- Vaccination: Discuss vaccination with your Family Doctor, as it may also reduce the risk of repeat outbreaks. It’s important to obtain up-to-date information about new vaccine formulations that may be more effective in prevention. There are several vaccines available, and recommendations may change as new research findings emerge.
A comprehensive approach to the treatment and prevention of shingles can significantly reduce the risk of complications and improve the quality of life for patients.
Blood tests can be performed to detect the presence and activity of Varicella Zoster Virus (VZV) at Armin Labs, Germany.
Conclusion
Herpes zoster, commonly known as shingles, is a viral infection caused by the varicella-zoster virus. It can lead to significant health complications if not managed properly. Understanding its transmission and prevention strategies, including vaccination and maintaining a healthy lifestyle, is crucial to minimizing the risk of flare-ups and complications. Effective treatments, such as antiviral medications and pain relievers, help alleviate symptoms and promote healing. A comprehensive approach to treatment and prevention can significantly enhance the quality of life for patients and prevent serious long-term effects.
