NAFLD: The Largest Hidden Consequence of Chronic Insulin Resistance
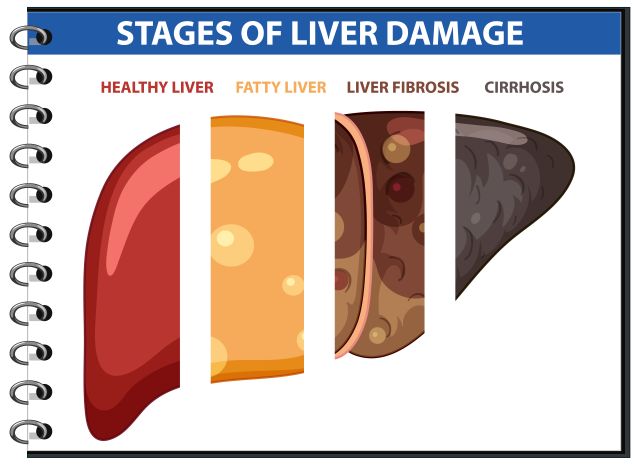
Diagnosis “fatty liver” is now increasingly detected incidentally-during ultrasound, CT, or MRI examinations performed for other reasons. It is found in people of different ages, body types, and lifestyles, often in the complete absence of pain, pronounced complaints, or abnormalities in standard blood tests.









